In this article, Nigel Zoltie, Accident & Emergency consultant and medicolegal expert, examines the latest NHS Resolution and Royal College of Emergency Medicine review into the most common causes of clinical negligence claims in emergency medicine. He outlines the recurring issues identified, from diagnostic errors and delayed care to missed fractures and pressure sore management and explains how their methodology offers a clear framework for medicolegal experts assessing breaches of duty in complex acute cases.
The latest report from NHS Resolution highlighted emergency medicine as one of the top causes of clinical negligence claims. The analysis by NHSR and the Royal College of Emergency Medicine offers a framework for understanding the causes of claims. In turn, that provides a valuable methodology for the medicolegal expert witness who is instructed to opine on the question of whether there was a breach of duty and, if so, by whom.
Introduction
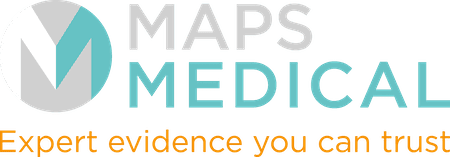
In the most recent report from NHS Resolution (2025 report including figures up to 2024), Emergency Medicine is one of the top “offenders” for clinical negligence claims. The chart below shows the top four categories of notifications.
The number of claims is demonstrated in graphical detail below:
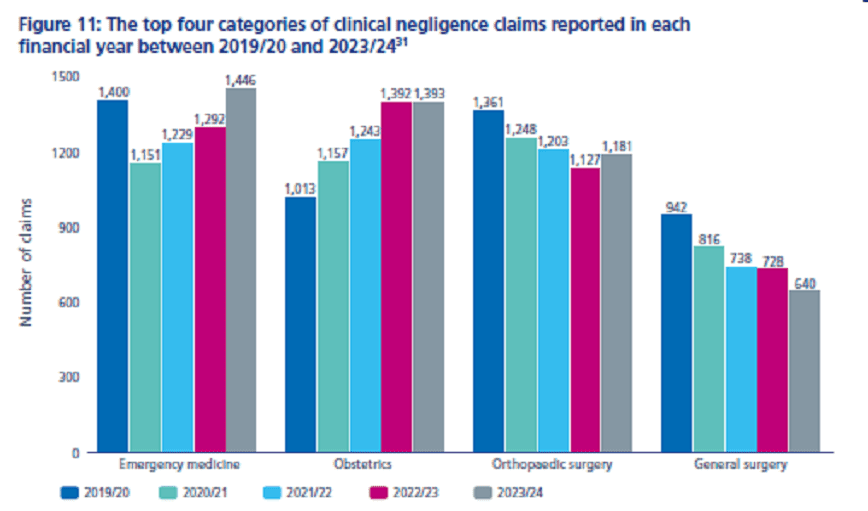
This shows that, where a speciality is known, Emergency Medicine claims number the most, even outnumbering obstetric claims.
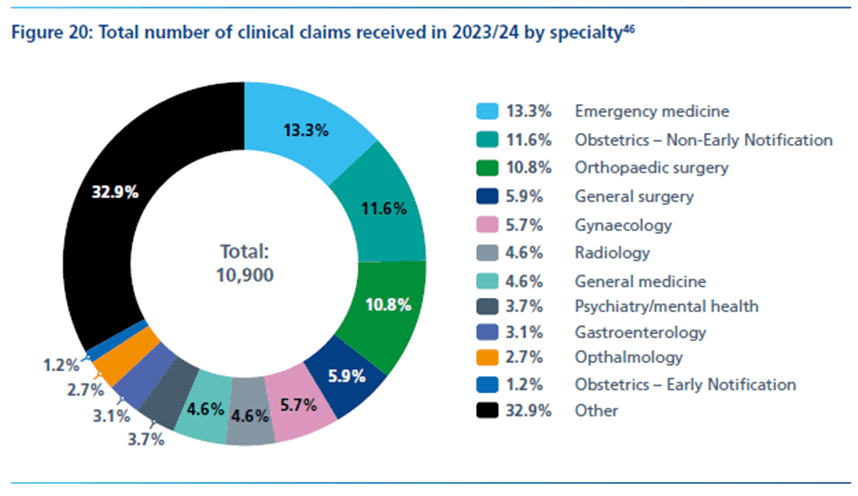
When it comes to the value of claims, Emergency Medicine falls behind obstetrics, as the diagram below shows.
This is perhaps unsurprising, with the value of successful birth claims spiralling.
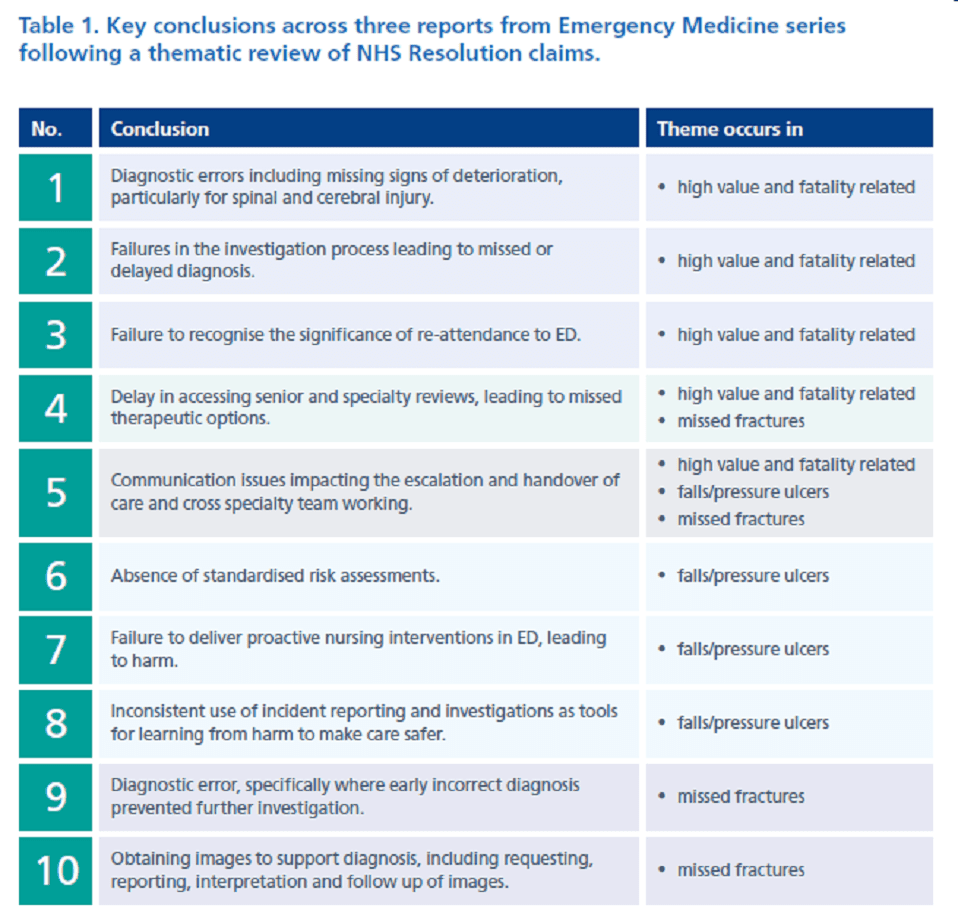
A review by NHS Resolution and the Royal College of Emergency Medicine identified three grouped areas of concern. They produced a report on each of these three areas, with themes identified as to where the problems lay. The table is reproduced below.
High value and fatality related claims
These cases included those where clinical errors in the Emergency Department resulted in a sequence of events leading to high value claims (eg missed opportunity to treat stroke, missed Cauda Equina syndrome, delay in treating sepsis – all causing life-changing circumstances). Several general factors were identified:
- Diagnostic error – missed signs of deterioration and failure to investigate; and missed, incorrect and delayed diagnosis. Contributing factors to diagnostic failure included:
- Problems with history taking.
- Too high a threshold for arranging a definitive diagnostic investigation to confirm or refute a suspected or possible severe condition.
- Incorrect weighting of history and findings, particularly the significance of severe pain.
- Important negatives not documented.
- Potential confounding factors not recognised.
- Inadequate or misdirected physical examination.
- Poor documentation.
- All of these appear to occur more frequently in respect of patients admitted to an inappropriate or non-standard area of the ED.
- Failure to recognise the significance of repeat attendance
- A patient presenting to the ED on several occasions is unlikely to see the same clinician each time and this is particularly problematic for patients with repeat attendances across care providers, sometimes in different sites and to different specialties within secondary care. If the patient presents to different EDs and different primary care settings, the significance of these repeated visits can be further lost. Repeat attendance should be recognised as a red flag.
- Delays in care
- Delay accessing diagnostic services.
- Delay accessing specialist opinion.
- Delays with transfer.
- Delay resulting in missed therapeutic options.
- Problems with communication, escalation and cross speciality working
- Failure to access information provided in GP letter, ambulance sheet or triage notes.
- Failure to recognise deterioration.
- Failure to escalate.
- Limited or incorrect information provided when escalating care to a senior ED doctor or other specialist.
Missed fractures
The following themes were identified as contributory factors to claims relating to missed fractures:
- Diagnostic error, specifically where early incorrect diagnosis prevented further investigation.
- Obtaining images to support diagnosis, including requesting, reporting, interpretation and follow-up of images.
- Communication, team working and escalation.
- Delays in care, including specialty reviews and missed therapeutic options.
Contributing factors to claims relating to missed fracture included:
- problems with history taking.
- clinical assessment and examination.
- competence of practitioner for clinical examination.
- ensuring EM clinicians hold the sufficient skills and knowledge, training, supervision and support.
Pressure sores and ulcers
This may be an unexpected problem identified as a result of Emergency Department care. However, as patients presenting are generally more unwell than in the past, and the wait for ward beds becomes longer, those ill and infirm patients, at high risk of pressure sores and ulcers, spend longer on hard Emergency Department trolleys, in corridors, with all but the most basic of care (and sometimes not even that). The medical care and interventions may be open to medicolegal discussion as to who has the duty of care, and whether it was provided properly, but the nursing care is without doubt provided by the Emergency Department nurses.
The best management of pressure sores and ulcers is prevention, and this starts as soon as the patient arrives in the Emergency Department. There is therefore a drive within Emergency Departments to initiate risk assessments and provide the appropriate preventative measures.
This problem would, of course, be alleviated if there were no waits for ward beds for admissions waiting in the Emergency Department (we can all wish!).
What can other medicolegal experts learn from this?
In many medicolegal reviews, it becomes obvious that some failures have occurred, and the medicolegal expert has to attempt to identify where the standard of care was below a reasonable standard. The methodology of the above reviews offers a very useful structure to allow identification of where the care was below standard, especially in a typical complex acute situation.
Was the failure a:
- Diagnostic error due to:
- Problems with history taking?
- Too high a threshold for arranging a definitive diagnostic investigation to confirm or refute a suspected or possible severe condition?
- Incorrect weighting of history and findings, particularly the significance of severe pain?
- Important negatives not documented?
- Potential confounding factors not recognised?
- Inadequate or misdirected physical examination?
- Poor documentation?
Or was the failure due to:
- Delays in care due to:
- Delay accessing diagnostic services.
- Delay accessing further specialist opinion.
- Delays with transfer.
- Delay resulting in missed therapeutic options.
Or was the failure due to:
- Problems with communication, escalation and cross-speciality working such as:
- Failure to provide appropriate information to another clinician.
- Failure to access information provided by another clinician.
- Failure to recognise deterioration over time.
- Failure to escalate.
The above framework may assist all medicolegal experts in their approach to identifying where the main component of a breach of duty may occur, or commonly where there were several components of breach. It may also help in identifying the person or team to whom the duty of care fell, and therefore who is responsible for the breach.
The clearer a medicolegal report is, the easier it is for the legal team to understand the concepts and I commend the above thought process for all medicolegal experts to consider as part of their general approach to breach of duty reports.